Over the past weekend, VanRamblings had the opportunity to speak with a senior member of British Columbia’s public health pandemic response team, and the information with which we were provided was hopeful for B.C.’s near term future.
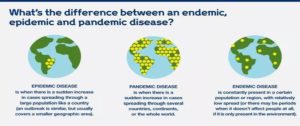
“British Columbia has entered the endemic phase of what we’ve all come to know as the pandemic this past 19 months, in fact, some while ago,” our unnamed source, unauthorized to speak on behalf of the office of British Columbia’s Public Health Office, told VanRamblings. “We’re not far off from removing mask mandates in those areas of the province where the full vaccination rate exceeds 90%, as is the case in Vancouver city proper, where the rate of fully vaccinated persons is currently 95% plus. Other regions of the province — Fraser Valley East, the Interior and Northern Health — have a ways to go before mask mandates, and other restrictions are removed by British Columbia’s public health office.”
VanRamblings asked the individual with whom we spoke about the current high COVID-19 infection rates we’re experiencing in British Columbia — most recently, the 3rd highest in Canada — and how this phenomenon might be accounted for …
“In British Columbia, we’re experiencing a series of super spreader events brought on by the unvaccinated members of regional communities, mostly situated in the three regions of the province where vaccination rates are low. Fully 98% of all COVID-19 hospitalizations and admissions to hospital ICU’s has occurred either within the unvaccinated community, or resultant from vulnerable vaccinated persons coming into contact with unvaccinated persons,” avers our public health source.
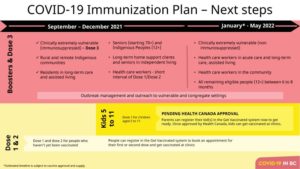
VanRamblings was told that in all likelihood British Columbians will be out of the worst of COVID-19 — even given the current and deadly virulence of the Delta variant — by early spring 2022, when life will return to some sense of “normal”, as we’ve all been observing now with capacity restrictions being lifted at Vancouver Canucks home games, within movie theatre complexes, and even at concerts.
When we asked our source about the 327 doctors, nurses and other health care professionals in British Columbia who have yet to get their first mRNA vaccine dose, our source simply rolled their eyes, muttering …
“As a health care professional, you are a scientist. Why you wouldn’t acknowledge the science on vaccines is beyond me? To say the least, that unfortunate development is disappointing, for those of us in the profession, and for all British Columbians.”
Or, as British Columbia Public Health Officer Dr. Bonnie Henry stated on Monday …
Health care is "probably not the right profession" for workers who don't recognize the importance of vaccines, Dr. Bonnie Henry said Monday.
3,325 health-care workers in B.C. — 2.6 per cent of the work force — are unvaccinated and on unpaid leave. https://t.co/tmuoWGWyYx pic.twitter.com/kYMaqyWxOI
— CBC British Columbia (@cbcnewsbc) November 1, 2021
On balance, it is probable that the comfort level for most of us in the general public will not be alleviated until infection, hospitalization and ICU rates are observed as being significantly reduced, with COVID-19 death rates all but eliminated on most reporting days, and the rate of death from COVID-19 in B.C. minimal at worst.